[News] Shanghai hospital successfully treated a critically ill patient with aortic valve disease
- Robert Cai

- Aug 13, 2025
- 10 min read

According to [Outpatient Clinic] magazine, a team led by Director Guo Zhifu of the Department of Cardiology at Shanghai Changhai Hospital, along with Professors Zhu Ni, Bai Yuan, and Zhu Jiaqi, recently performed a TAVR procedure using the VenusA-Pro® transcatheter aortic valve retrievable delivery system, supported by ECMO, on a critically ill patient with severe aortic stenosis and severe regurgitation. The patient suffered from recurrent acute left ventricular failure and multi-organ dysfunction, poor underlying health, and high surgical risk. Furthermore, the complex anatomy of the aortic valve posed a significant challenge. Following thorough preoperative evaluation, imaging analysis, and MDT, the valve center team collaborated on the day of surgery to successfully and accurately implant the valve. Immediately after the procedure, transesophageal ultrasound revealed no central regurgitation, confirming the success of the procedure. This procedure offers new treatment options and hope for patients with severe bicuspid valve calcification and severe heart failure, and we hope it will benefit more critically ill AS patients.
Case Information
Basic Information: A 74-year-old male patient weighing 80 kg.
Current Complaints: Chest tightness and shortness of breath for two months, bilateral lower limb edema for 10 days, which worsened and resulted in inability to lie flat for three days.
Current Medical History: Two months prior, the patient developed chest tightness, fatigue, palpitations, and paroxysmal nocturnal dyspnea after exertion, accompanied by fatigue, nausea, abdominal distension, and loss of appetite, which resolved with rest. Bilateral lower limb edema developed over 10 days prior, and worsened three days prior. He presented with no diarrhea, hematemesis, melena, headache, or dizziness, and these symptoms gradually resolved despite rest. Despite receiving appropriate treatment, his symptoms persisted. To further clarify the diagnosis and treatment, he was admitted to our outpatient department with aortic stenosis.
Patient History: Lower limb fracture fixation 25 years prior; hypertension for four years, peaking at 190/110 mmHg; cerebral hemorrhage three years prior, treated conservatively; no history of diabetes.
Initial diagnosis: Valvular heart disease: severe aortic stenosis with severe regurgitation; relative mitral stenosis; severe tricuspid regurgitation; frequent premature ventricular contractions; heart function class IV (NYHA classification).
Preoperative Examination
Pulmonary function: extremely severe restrictive ventricular dysfunction.
Electrocardiogram: frequent premature ventricular contractions.
Echocardiogram: severe aortic stenosis (valve area 0.8 cm², peak velocity 529 cm/s, pressure gradient 111 mmHg, mean velocity 387 cm/s, pressure gradient 65 mmHg) with severe regurgitation (instantaneous volume 36 ml); ascending aorta dilatation (aortic annulus diameter 2.3 cm, sinus 4.2 cm, widest aorta 4.3 cm); relative mitral stenosis; severe tricuspid regurgitation; global heart enlargement; decreased left ventricular systolic function (FS 19%, EF 38%).
STS score: 8.39%.
CT Assessment
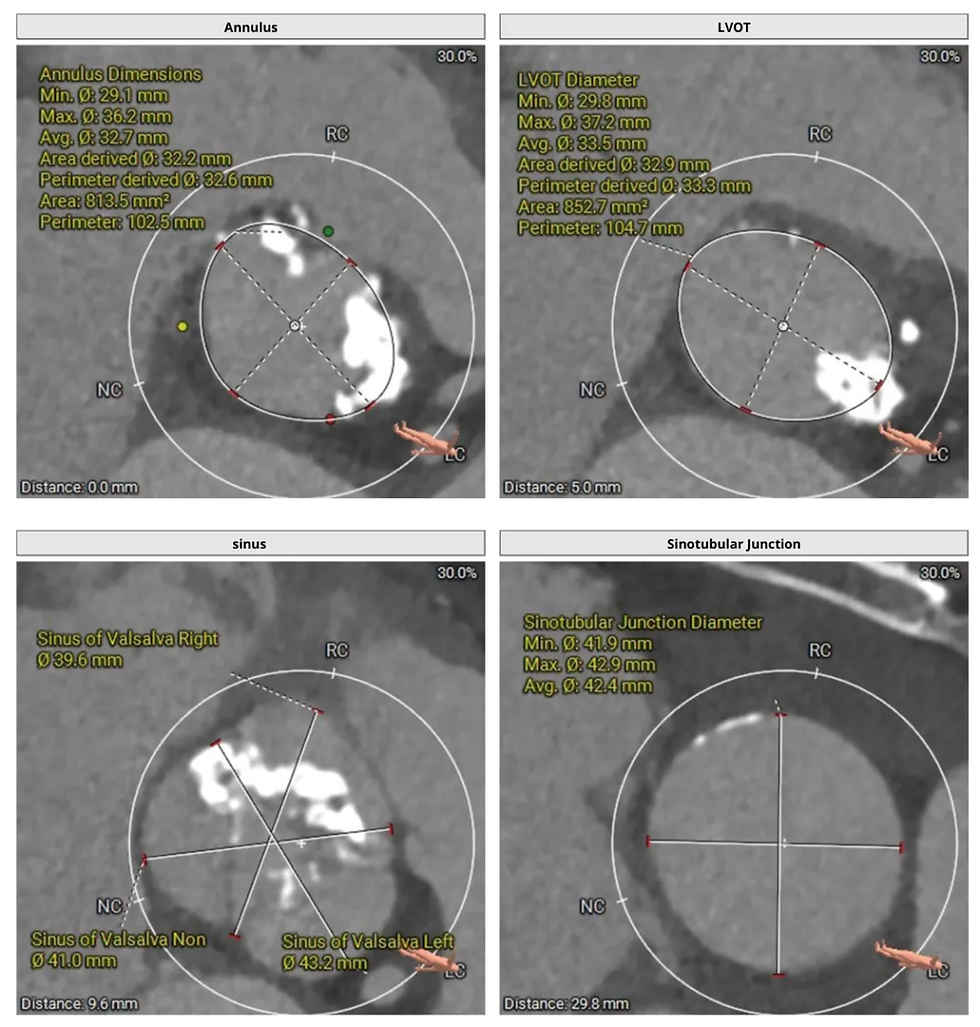
Type I bicuspid valve, left and right fusion, no visible partial fusion on the right, extremely severe calcification (calcification score 2047 mm³), calcification visible at the annular level, extending into the left ventricular outflow tract, large French sinus structure, left coronary ostium height approximately 13.2 mm, right coronary ostium height approximately 20.2 mm, STJ height approximately 29.8 mm, diameter approximately 42.4 mm, widening of the ascending aorta approximately 43.7 mm at its widest point, cardiac angle approximately 53°.





Strategy Development
Type I bicuspid valve, left and right fusion, no visible partial fusion on the right, extremely severe calcification, calcification visible at the annular level, extending into the left ventricular outflow tract, large French sinus structure, both leaflets length below the inferior margin of the coronary artery ostium, low coronary risk. VenusA-Valve L32 was implanted under general anesthesia and ECMO support via the right femoral artery as the primary approach. Predilation was not performed for better anchoring. Type I bicuspid valve will have a step-like bulge. The right leaflet has no lifting effect, making it slightly difficult to cross the valve. Pay attention to the depth of the guidewire insertion throughout the whole process to prevent the guidewire from slipping out of the left ventricle. Pay attention to the tension of the guidewire.
Operational Procedure
During the operation, the right radial artery was punctured under general anesthesia. Coronary angiography showed no obvious stenosis of the left main coronary artery, left circumflex artery, left anterior descending artery, and right coronary artery. ECMO arteriovenous sheath was inserted through the left femoral artery and femoral vein. An 8F sheath was inserted into the right femoral artery. Two vascular suture devices were pre-placed. A 0.035 straight loach guidewire was passed through the aortic valve orifice to the left ventricle. The pigtail catheter was replaced to measure the left ventricular pressure of 202/15 (77) mmHg and the aortic root pressure of 96/50 (66) mmHg. The super-rigid guidewire was exchanged to the apex of the heart, and the VenusA-Pro valve system was inserted into the appropriate position of the aortic valve. The extracorporeal circulation was clamped to reduce the blood pressure to 50/30 mmHg. The valve was slowly released to restore circulation. The pigtail catheter was reinserted into the left ventricle. The left ventricular pressure was 127/0 (42) mmHg, and the aortic root pressure was 108/48 (68) mmHg. Aortic root angiography showed good imaging of the left and right coronary arteries, no paravalvular leak and central regurgitation. The ECMO flow was gradually reduced. The patient's blood pressure stabilized at 137/48 mmHg. A temporary pacemaker was inserted, the auxiliary catheter and guidewire were removed, and the blood vessels were sutured. The operation was successfully completed. Postoperative echocardiography showed that the aortic valve intervention valve echo was normal, opening and closing were normal, there was no regurgitation at the valve orifice, and no paravalvular leak was found.









Summary
This patient presented with a Type I bicuspid valve with severe stenosis and severe regurgitation, combined with extremely severe calcification. Furthermore, the patient suffered recurrent acute left heart failure and multi-organ dysfunction, with an STS score of 8.39%, placing him in a very high-risk surgical population and posing a high risk for traditional surgery. Based on the patient's condition, the surgical team performed TAVR with ECMO support. Preoperatively, multimodal imaging was used to accurately assess valve morphology, calcification distribution, and access conditions. During the procedure, no pre-dilation was chosen to minimize the risk of calcification dislodgement. A "slow-fast-slow" release rhythm was employed to ensure precise valve positioning. The ECMO system maintained hemodynamic stability and minimized the risk of intraoperative circulatory collapse. The success of the surgery not only demonstrates the efficient and close multidisciplinary collaboration of the team, but also demonstrates the clinical value of the VenusA-Pro valve in complex anatomies. It provides valuable guidance for clinical decision-making in patients with extremely severe bicuspid valve calcification and severe heart failure. We look forward to seeing more similar patients gain new life through TAVR in the future.

Expert Profile

Director of the Department of Cardiology at Shanghai Changhai Hospital, Chief Physician, Professor, Doctor of Medicine, and Doctoral Supervisor. He is recognized as an Outstanding Academic Leader in Shanghai, a Young Science and Technology Rising Star in Shanghai, and an Outstanding Young Medical Talent in Shanghai's "Medical Garden Rising Star." He was selected for the Naval Medical University's Deep Blue Talent Project Pilot Program. He has served as a member of the Chinese Medical Association's Cardiology Committee, a member of the Arrhythmia Group of the Chinese Medical Association's Cardiology Branch, a member of the Shanghai Medical Association's Internal Medicine Branch, a member of the Cardiology Committee of the Shanghai Biomedical Engineering Society, a Young Member of the Cardiology Branch of the Shanghai Medical Association, Secretary of the Congenital Heart Disease Working Group and Member of the Arrhythmia Working Group of the PLA Cardiovascular Disease Interventional Diagnosis and Treatment Quality Control Committee, an instructor at the National Cardiovascular Disease Interventional Diagnosis and Treatment Technology Training Base, a correspondence reviewer for the National Natural Science Foundation of China, a graduate thesis reviewer for the Ministry of Education's Degree Center, a member of the Shanghai Science and Technology Expert Database, a reviewer for Peptides, JEI, Islets, and CDR, and a reviewer for the TCT Conference in the United States. She has been recognized as an Advanced Teaching Individual at the University, an Outstanding Communist Party Member of the Hospital, one of the Hospital's Top Ten Outstanding Clinical Physicians, an Outstanding Young Scientist in Science and Technology, and an Outstanding Instructor for Shanghai's Standardized Resident Physician Training Program. She was also awarded the "May Fourth Youth Medal" by the Shanghai Municipal Health and Family Planning Commission and received a Third-Class Merit. Her research achievements include being the first applicant for two National Natural Science Foundation of China grants, four Shanghai Municipal Foundation grants, and one grant from the Central Military Commission's Logistics Department. She has published 15 SCI-indexed papers as the first/corresponding author, with the highest single-paper impact factor of 23.213, and one of her papers has been recognized as one of China's 100 Most Influential International Academic Papers. She is the first applicant for one national invention patent and has edited one monograph.

Doctor of Medicine, Postdoctoral Fellow at Thomas Jefferson University School of Medicine. She is an Associate Chief Physician, Associate Professor, Master's Supervisor, and Supervisor for Standardized Resident Physician Training in the Department of Cardiology at Shanghai Changhai Hospital. He is a member of the Asia-Pacific Structural Heart Disease Youth Club; the Structural Heart Disease Professional Committee of the China Association for Health and Technology Promotion; the Chinese Cardiovascular Physician Innovation Club; the Youth Work Committee of the Shanghai Stroke Society; the Structural and Valvular Center Working Group of the Cardiovascular Branch of the Shanghai Medical Association; the Pulmonary Circulation Group of the Cardiovascular Disease Branch of the Shanghai Medical Association; a member of the Shanghai Science and Technology Expert Database; and a reviewer for SCI journals such as Genes Dis. He has received numerous talent programs and awards, including the 2023 Paul Dudley White International Scholar Award from the American Heart Association, the Shanghai Young and Middle-aged Teachers Overseas Visiting Program for General Colleges and Universities, the Second Military Medical University Outstanding Civilian Position Allowance, the "Four-Have" Outstanding Civilian, and the title of Outstanding Grassroots Cadre of Changhai Hospital. As the principal investigator, he received the Shanghai Medical Science and Technology Achievement Promotion Award and the Shanghai Medical Science and Technology Third Prize. As the project leader, he has overseen five research projects, including those funded by the National Natural Science Foundation of China. He has been granted one invention patent and two utility model patents. He has published over ten SCI papers, with the highest single-paper impact factor of 10.9 and the highest single-paper citation of nearly 300 times (ESI Highly Cited Paper).

Deputy Director, Associate Chief Physician, Associate Professor, Master's Supervisor, and Resident Instructor of the Department of Cardiology at Shanghai Changhai Hospital.
Member of the Structural Heart Disease Section of the Chinese Medical Association's Cardiovascular Disease Branch, Vice Chairman of the Structural Heart Disease Professional Committee of the Chinese Association for the Promotion of Human Health Science and Technology, member of the Left Atrial Appendage Closure Study Group of the Cardiac Rhythmology Branch of the Chinese Society of Biomedical Engineering, member of the First Left Atrial Appendage Closure Working Committee of the China Atrial Fibrillation Center Alliance, Young Member of the Chinese Cardiovascular Innovation Club (CCI), Gold Member of the Asia-Pacific Structural Heart Youth Club, Expert of the Shanghai Atrial Fibrillation Alliance Training Expert Group, and member of the Congenital Heart Disease and Structural Heart Disease Intervention Working Group of the Fourth Committee of the PLA Cardiovascular Disease Interventional Diagnosis and Treatment Quality Control Committee.
He has long been engaged in the diagnosis and treatment of cardiovascular diseases, with structural heart disease and coronary artery disease intervention as his main areas of expertise. In 2017, he studied cardiovascular interventional technology at the H-G-W Hospital in Germany. He has been awarded the Third Class Merit once, and has been recognized as an Outstanding Instructor for National Resident Training Programs, an Outstanding Instructor for Shanghai Resident Training Programs, and a Wu Mengchao-style Outstanding Young Person of the Second Military Medical University. He has also received the Second Class Shanghai Medical Science and Technology Award and the Second Class Military Science and Technology Progress Award. He has co-edited over 30 monographs, published over 50 papers, and holds five authorized patents.

He is an Associate Chief Physician, Associate Professor, and Graduate Supervisor in the Department of Cardiology at the First Affiliated Hospital of the Naval Medical University (Shanghai Changhai Hospital). He specializes in interventional therapy for complex coronary heart disease. In recent years, he has focused on minimally invasive treatments for valvular heart disease, including left atrial appendage closure for atrial fibrillation and patent foramen ovale closure. He performs over 400 interventions annually. He has presided over nine grants, including those from the National Natural Science Foundation of China, the Shanghai Natural Science Foundation, the Chinese Medical Association, and other institutions. He has presented his work at numerous national academic conferences. He has received the Third Class Shanghai Medical Progress Award, the Second Class Military Teaching Achievement Award, and three utility model patents. He currently serves as a Young Committee Member of the Chinese Medical Association's Geriatrics Branch, a Young Committee Member of the PLA Geriatrics Society, a member of the Shanghai Medical Association's Blood Lipids and Atherosclerosis Group, and a member of the Navy Innovation Team. He has been awarded the Third Class Merit twice and the Third Class Merit once. He was recognized as one of the 100 Most Influential International Papers in China in 2011, an "A-Level Teacher" at the university in 2012, a "Teaching Model" at the former General Logistics Department's University Teaching Competition in 2013, one of the "Top Ten Outstanding Clinical Physicians" at the hospital in 2014, and a "Future Star" of the Chinese Medical Doctor Association's Cardiovascular Branch in 2015. From 2019 to 2020, he was a visiting scholar at the Center for Translational Medicine at Thomas Jefferson Medical College in Philadelphia and the DeBakey Cardiovascular Intervention Center at Methodist Hospital in Houston. In 2021, he served as an acting academic leader in cardiology at the Second Naval Hospital of the Southern Theater Command, where he developed numerous new clinical technologies. He is a Silver Qing member of the Asia-Pacific Structural Heart Disease Youth Club in 2022 and runner-up in the 2024 AP-SHD National Elite Competition. He participated in the editing of 10 teaching aids, published 12 SCI papers, and published a clinical paper in the European Heart Journal with the highest impact factor of 43 points. He was cited more than 1,400 times.
If you have a family member or friend who needs to come to China to receive treatment from the excellent medical teams mentioned above, or if you are interested in establishing a long-term referral partnership, please first browse REBIO GROUP's cross-border healthcare services and then contact our professional team.
REBIO GROUP is dedicated to providing convenient and worry-free, world-class Chinese healthcare services to international patients. We are your trusted partner, handling every detail with professionalism and care.
![[Insight] The ALICE Threshold: America's Quiet Economic Divide Under SaaS Society](https://static.wixstatic.com/media/100ece_b85be5890d4b4ba99c118cbfca1cd9f7~mv2.jpg/v1/fill/w_892,h_502,al_c,q_85,enc_avif,quality_auto/100ece_b85be5890d4b4ba99c118cbfca1cd9f7~mv2.jpg)


Comments